Mastectomy is removal of the breast. Other nearby tissue may also be removed if it appears that cancer may have spread to these areas.
All mastectomies remove the whole breast. Because the size and location of tumors and where the cancer might have spread differ from one person to another, the amount of other tissue removed during surgery also varies.
Mastectomy procedures include:
Male breast cancer is usually treated with one of the mastectomy procedures.
Depending on the location of the tumor in the breast or other factors, you may be able to have a skin-sparing or nipple-sparing mastectomy.
- Skin-sparing mastectomy leaves most of the skin that was over the breast, except for the nipple and the areola.
- Nipple-sparing mastectomy saves the skin over the breast as well as the nipple and areola.
If you'd like, you might choose to have breast reconstruction after a mastectomy. Reconstruction can be done during the same surgery as the mastectomy. Or it may be done later as a separate procedure.
What to expect
After your surgery, you will be taken to a recovery room. A nurse will be able to help with any nausea, pain, or anxiety you might have.
When you wake up from surgery, you will have a bandage over the surgery site. You will also have one or two drainage tubes to collect fluid and keep it from building up around the surgery area. You will be taught how to care for the drains at home.
Your doctor or nurse will give you instructions on pain control and caring for your incision. Follow your doctor's instructions about when you can take a shower or bath.
Most people go home within 24 hours after a mastectomy. If you have breast reconstruction during the same surgery, you may be in the hospital longer.
A physical therapist may show you exercises while you are still in the hospital. These should help keep your shoulder from getting stiff. You will need to avoid strenuous activity for several weeks. Your doctor will let you know how soon you can increase your activity level.
Why It Is Done
Mastectomy is done to remove the breast. It's usually done to help treat or prevent breast cancer.
How Well It Works
For early-stage breast cancer, breast-conserving surgery (lumpectomy) along with radiation therapy has the same survival rate as mastectomy. But many people still have a mastectomy, even though it is a more extensive surgery.
Having a mastectomy instead of a lumpectomy followed by radiation does not lower the chance that cancer will come back in the same area. The chance that breast cancer will come back in the same area or breast is about the same.
Some people choose a mastectomy to avoid radiation. But sometimes radiation is needed after a mastectomy.
People with metastatic breast cancer do not usually have surgery. Survival is not likely to be increased by having surgery.
Risks
Like any surgery, both mastectomy and breast-conserving surgery have risks. Possible problems from breast surgery include:
- Breast pain or pulling, pinching, tingling, or numbness.
- Buildup of blood or clear fluid in the wound.
- General surgery risks. These include infection, bleeding, poor wound healing, and a reaction to the anesthesia used in surgery.
If lymph nodes under the arm were removed, possible problems include:
- Swelling of the arm (lymphedema).
- Numbness in the area where lymph nodes were removed.
Credits
Current as of: October 1, 2025
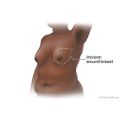 Mastectomy
Mastectomy  Breast surgery: Modified radical mastectomy
Breast surgery: Modified radical mastectomy  Axillary lymph nodes
Axillary lymph nodes  Skin-sparing mastectomy with teardrop cut
Skin-sparing mastectomy with teardrop cut 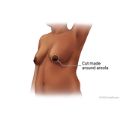 Skin-sparing mastectomy with periareolar cut
Skin-sparing mastectomy with periareolar cut  Nipple-sparing mastectomy with periareolar cut
Nipple-sparing mastectomy with periareolar cut 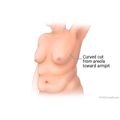 Nipple-sparing mastectomy with lateral cut
Nipple-sparing mastectomy with lateral cut 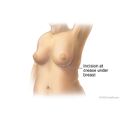 Nipple-sparing mastectomy with inframammary cut
Nipple-sparing mastectomy with inframammary cut 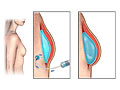 Breast Implant After Mastectomy
Breast Implant After Mastectomy 


